HPV
Human Papillomavirus (HPV) is the most common STI in the United States but perhaps one of the most misunderstood. To prepare you to talk with young people about HPV, we’ve got the answers to their most frequently asked questions.
Frequently Asked Questions
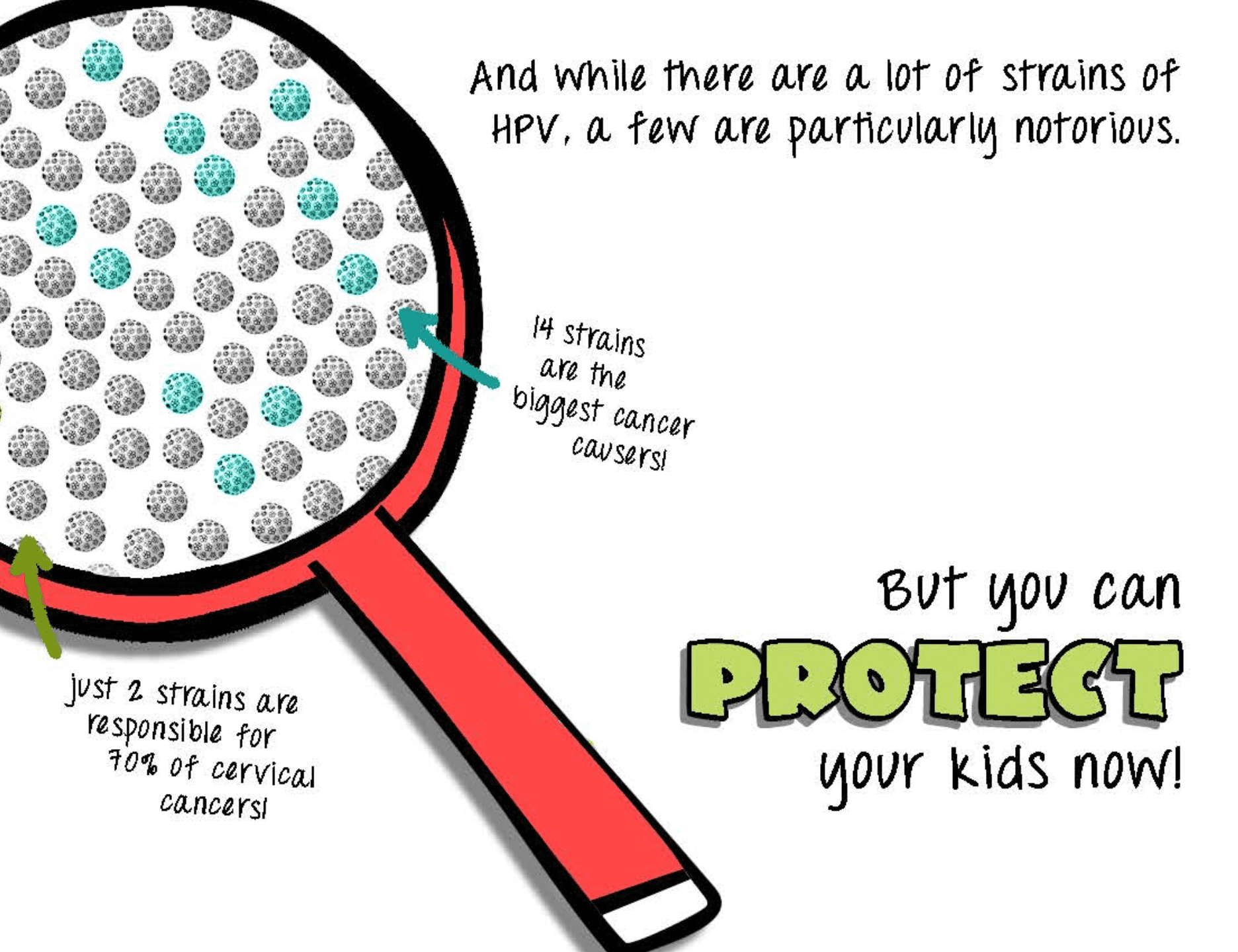
Human Papillomavirus, or HPV, is a group of more than 200 viruses, of which around 40 are spread through sexual contact.
While in most cases HPV goes away on its own, it can cause health problems, such as genital warts. Genital warts are soft bumps that appear on the genitals; they may form as a single bump or cluster of bumps. They can vary in shape and size and typically cause itching and discomfort.
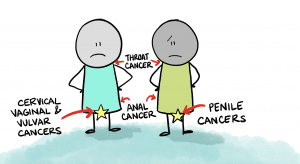
HPV can also cause cervical, vulvar, and vaginal cancer in people with a cervix, vulva, and vagina, and penile cancer in people with a penis. Anal and oropharyngeal cancer (cancer of the back of the throat and tonsils) can happen to anyone.
Every year, thousands of people are affected by cancers caused by HPV.
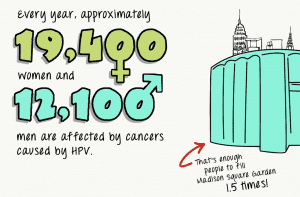
There are nearly 14 million new cases of HPV diagnosed every year. Young adults between the ages of 15 and 24 account for nearly 50% of HPV diagnoses. In fact, it is estimated that 8 out of 10 people will get HPV at some point in their lives.
HPV is transmitted through vaginal, anal, or oral sex with someone who has the virus. HPV can be spread even if a person shows no signs or symptoms of infection. It is also possible to develop symptoms years after having sexual intercourse with an infected person, making it difficult to know when you first became infected with the virus. This is why it is important to learn about the correct and consistent use of latex condoms, nitrile internal condoms, and dental dams to prevent the transmission of HPV during sexual intercourse.
Unlike most STIs, such as chlamydia or gonorrhea, there is currently no official test for HPV.
A healthcare provider may be able to provide a diagnosis by conducting a Pap smear, or by using an acetic acid (vinegar) solution test on any growths that may be genital warts. (A positive genital warts test would indicate a person has HPV, but it is not considered an HPV test because not everyone who has HPV gets genital warts.)
For people with a uterus, HPV is often diagnosed through an abnormal Pap smear.
Gardasil 9 is the only vaccine licensed by the FDA for use in the United States to prevent HPV.
The CDC recommends HPV vaccination at 11 or 12 years of age. Unlike other sexual health services, parental consent is required for vaccination of any child under the age of 18.
The HPV vaccine requires three doses if you get vaccinated after age 15, and two doses if you complete the vaccine series before you turn 15.
According to recent data, 78.9% of vaccine-eligible teens ages 13-17 in Maryland, for example, initiated the HPV vaccine series compared to 71.5% of teens in the U.S.

The HPV vaccine may be available at a doctor’s office, local community health clinics, health departments, or school-based health centers.
If the young person’s health insurance does not cover the cost of the vaccine or they do not have health insurance, they may be eligible to get the vaccine for free through the Vaccine for Children Program, which offers no-cost vaccines for Medicaid eligible, uninsured, underinsured, and American Indian or Alaskan Native children under the age of 18.
The research is clear—the HPV vaccine is safe and effective.
While there’s a lot of misinformation about vaccines out there, the truth is, the side effects of HPV vaccines are mild and may include pain at the injection site, fever, dizziness, and fainting.
Unfortunately, no, there is no cure for HPV, which is why it is important to practice safe sex, limit the number of sexual partners, and, if possible, complete the HPV vaccine series.
We strongly encourage young people to have a conversation with their healthcare provider and their parents/caregiver/trusted adult about the HPV vaccine.
This resource from Do Something provides talking points for young people to have a conversation with their parents about the HPV vaccine.
Contributing Staff